The Intricacies of the Inner Ear: How Sensorineural Hearing Loss Occurs
The Anatomy of the Auditory System: A Deep Dive
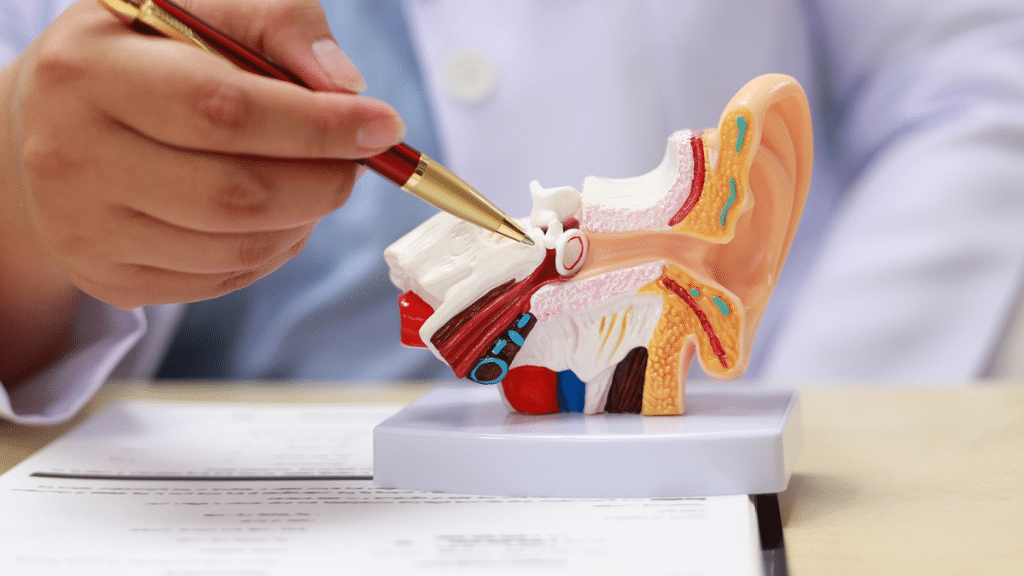
The auditory system is a remarkable biological marvel, designed to convert sound waves into electrical signals that the brain interprets as sound. The journey begins in the outer ear, where sound waves are captured, channeled through the ear canal, and vibrate the eardrum. These vibrations then travel through the middle ear, where three tiny bones—the malleus, incus, and stapes—amplify the sound. The real magic, however, occurs in the inner ear. Here lies the cochlea, a spiral-shaped organ filled with fluid and lined with thousands of hair cells. These hair cells play a crucial role in sensorineural hearing loss (SNHL); when stimulated by sound vibrations, they convert them into electrical impulses sent to the auditory nerve and, subsequently, to the brain.
In addition to the cochlea, the inner ear houses the vestibular system responsible for balance. The intricate anatomy of the auditory system means that any disruption or damage to the hair cells or auditory nerve can lead to sensorineural hearing loss, which is typically permanent. Understanding this complex interplay is essential when discussing the implications of SNHL, as it underscores the importance of protecting our ears and seeking early intervention for hearing issues.
What Triggered This Change? Common Causes of Sensorineural Hearing Loss
Sensorineural hearing loss can stem from various factors, each with distinct mechanisms that affect the auditory system. Ageing, known as presbycusis, is one of the most prevalent causes, usually beginning around the age of 60. As individuals age, hair cells in the cochlea naturally degenerate, impacting the ability to hear high-frequency sounds. Environmental factors, such as prolonged exposure to loud noises, can lead to noise-induced hearing loss, a growing concern among people in occupational environments such as construction or music. This type of SNHL often arises from damage to hair cells due to the intensity of sound, which is irreversible.
Genetic predisposition also plays a significant role in sensorineural hearing loss. Several hereditary conditions, such as Usher syndrome and Waardenburg syndrome, have been identified, highlighting the importance of family history in understanding one’s hearing health. Moreover, certain medical conditions—ranging from viral infections like mumps and measles to autoimmune diseases—can damage the auditory system. Ototoxic medications, especially certain antibiotics or chemotherapy agents, can also precipitate SNHL. Understanding these triggers can empower individuals to take proactive measures in consultation with healthcare professionals, identifying early warning signs, seeking genetic counseling, or adopting protective strategies in response to chronic noise exposure.
The Distinction Between Conductive and Sensorineural Loss: Why It Matters
When exploring hearing loss, it is essential to distinguish between conductive and sensorineural types, as this can significantly impact treatment approaches and outcomes. Conductive hearing loss occurs when sound cannot properly travel through the outer or middle ear due to blockages, fluid buildup, or structural defects. This type of hearing loss can often be temporary and reversible with medical or surgical intervention, such as treating ear infections or removing earwax.
In contrast, sensorineural hearing loss results from damage to the inner ear’s hair cells or the auditory nerve pathways. While conductive loss may sometimes lead to temporary solutions, SNHL usually involves permanent changes in the auditory system, focusing medical professionals on managing the condition rather than restoring hearing entirely. This distinction matters significantly in research and treatment options. It emphasizes the need for ongoing awareness and education about the roots and implications of hearing loss to ensure that individuals receive appropriate care and support tailored to their specific needs.
Diagnosing Sensorineural Hearing Loss: The Journey to Clarity
Understanding Audiometric Testing: Tools of the Trade
Diagnosing sensorineural hearing loss involves a series of comprehensive assessments, the cornerstone of which is audiometric testing. Audiologists employ a variety of methods to evaluate an individual’s hearing abilities, utilizing pure-tone audiometry, speech audiometry, and tympanometry. Pure-tone audiometry involves listening to pitch tones at various frequencies and volumes to establish the threshold at which sound is perceived. The results are depicted on an audiogram, providing visual confirmation of hearing loss severity and configuration.
Alongside pure-tone testing, speech audiometry assesses how well a person can understand speech, which is crucial for everyday communication. This test often involves repeated speech sounds at varying levels of loudness. Moreover, tympanometry evaluates the functioning of the middle ear by measuring the movement of the eardrum in response to air pressure changes. As a comprehensive suite of diagnostic tools, audiometric testing offers an effective and systemic means of determining both the presence and extent of sensorineural hearing loss, guiding further recommendations for treatment.
The Role of Imaging Tests: When Are They Necessary?
While audiometric tests provide critical insights into hearing capabilities, imaging tests such as computed tomography (CT) or magnetic resonance imaging (MRI) can be invaluable in diagnosing the underlying causes of sensorineural hearing loss. These imaging modalities can visualize the structures of the inner ear, identifying abnormalities such as tumors, malformations, or cholesteatoma that may require surgical intervention or specific medical management. Imaging can also help evaluate the auditory nerve’s integrity, ruling out issues like acoustic neuromas—benign tumors on the auditory nerve, which can lead to sensorineural hearing loss.
However, not every case of SNHL necessitates imaging studies; this decision is made based on patient history, audiometric results, and symptomatology. Understanding the appropriate context for these tests is crucial for patients and healthcare providers, as it can ensure a timely, accurate diagnosis and tailored treatment plan. While imaging tests may seem daunting, they are a fundamental component in formulating a comprehensive strategy for addressing sensorineural hearing loss effectively.
From Symptoms to Diagnosis: Recognizing the Signs Early
Recognizing early signs of sensorineural hearing loss can significantly affect the quality of life and management options available to individuals. Common symptoms include difficulty understanding speech in noisy environments, a sensation of muffled sounds, or the perception that others are mumbling. People may also notice an increase in their volume preferences for television or music, or they may frequently ask others to repeat themselves. If these symptoms persist, seeking an evaluation from an audiologist is imperative.
Routine hearing screenings are an excellent preventive measure for individuals at risk, including those with a family history of hearing loss or exposure to loud noises. Early diagnosis not only allows for more effective intervention strategies but can also lower the cognitive decline often associated with untreated hearing loss. Drawing attention to these symptoms and fostering an environment of communication about hearing health is crucial. Ultimately, the journey from recognizing symptoms to receiving a diagnosis is foundational in initiating appropriate treatments, leading to improved auditory experiences and quality of life.
Treatment Options: Navigating the Landscape of Hearing Restoration
Modern Hearing Aids: Technology at Your Fingertips
For many individuals with sensorineural hearing loss, hearing aids represent the most accessible and commonly utilized treatment option. Modern advancements in hearing aid technology have transformed these devices into highly sophisticated instruments capable of amplifying sounds while filtering out background noise, thus enhancing speech intelligibility. Available in various styles—from behind-the-ear to in-the-ear models—hearing aids are customizable to an individual’s specific hearing needs and lifestyle preferences.
Recent innovations, including digital signal processing and artificial intelligence, have allowed hearing aids to offer smart features such as automatic adjustments based on environmental cues and connectivity with smartphones and other devices. These enhancements not only improve the user experience but also encourage wider adoption among individuals of all ages. It is essential, however, to emphasize the importance of a professional fitting and ongoing audiological support to optimize hearing aids’ performance and ensure maximum benefit for each user.
Cochlear Implants: A Game-Changer for Severe Cases
For those with severe to profound sensorineural hearing loss, cochlear implants can offer a viable alternative when conventional hearing aids are no longer effective. A cochlear implant bypasses damaged hair cells in the cochlea, directly stimulating the auditory nerve through electrical impulses. This device consists of an external processor worn behind the ear and an internal implant surgically placed within the cochlea. The implications of cochlear implants are profound, often providing users with the opportunity to regain speech perception and improve communication abilities.
However, cochlear implants are not a one-size-fits-all solution. Candidates must undergo rigorous evaluation to determine suitability, considering factors such as the duration of hearing loss and overall health status. Also, post-implantation, users may undergo auditory training to maximize their benefits from the device. The impact on daily life after receiving a cochlear implant can be life-altering, allowing individuals to participate more fully in social interactions and contributing positively to emotional well-being and self-esteem.
Therapeutic Approaches: Exploring Audiology and Counseling
While technology plays a pivotal role in managing sensorineural hearing loss, therapeutic approaches such as audiology and counseling are equally essential. Audiologists not only fit hearing devices but also provide extensive education about hearing loss, strategies for communication, and auditory rehabilitation programs tailored to individual needs. Counseling can be critical for helping individuals and their families adjust to life with hearing loss, fostering coping strategies and enhancing interpersonal relationships.
Audiology services often include auditory training exercises designed to improve listening skills, auditory perception, and sound localization. Group therapy sessions can also serve as a valuable support network, offering opportunities to share experiences and strategies with peers facing similar challenges. Speech-language therapy may further aid individuals in developing effective communication techniques. The multifaceted approach to therapy addresses the psychological and social elements of living with sensorineural hearing loss, highlighting the importance of emotional support in conjunction with technical interventions.
Living with Sensorineural Hearing Loss: Embracing Adaptation and Support
Communicating with Confidence: Strategies for Everyday Interactions
Living with sensorineural hearing loss requires adaptation and effective communication strategies to foster confidence in daily interactions. It is vital for those affected to advocate for themselves by informing others about their hearing loss, which can enhance understanding and empathy. Simple modifications such as maintaining eye contact during conversations, utilizing clear speech, and choosing well-lit environments where lip-reading is possible can augment communication accuracy.
Moreover, technological aids play a significant role. For instance, utilizing captioning services during public presentations or using visual cues in conversations can bridge gaps in communication. Practicing patience and encouraging friends and family to engage in supportive dialogue can also help sustain interactions. Joining organizations that focus on communication strategies, such as the Hearing Loss Association of America (HLAA), can provide additional resources and support, empowering individuals to navigate social situations effectively while reducing anxiety associated with misunderstanding or miscommunication.
The Role of Support Groups and Resources: Finding Your Community
Support groups serve as a lifeline for individuals experiencing sensorineural hearing loss, promoting an environment of shared experiences and mutual understanding. Such organizations offer a platform for connecting with others facing similar challenges, reducing feelings of isolation. Through peer support and shared coping strategies, individuals often gain valuable insights that enhance their ability to manage their condition effectively.
Numerous resources are available, including local chapters of national organizations, online forums, and community programs geared towards those with hearing loss. Workshops and events focusing on topics like assistive listening devices, communication techniques, and emerging technologies can provide further education and empowerment. Building a robust support network not only aids in personal growth but can significantly enhance overall well-being, providing the encouragement and camaraderie essential for thriving despite the challenges of sensorineural hearing loss.
Innovations on the Horizon: Future Treatments and Research in Auditory Health
The future of treatment for sensorineural hearing loss is filled with promise, as ongoing research and technological innovations continue to evolve. Gene therapy, for instance, holds the potential to address genetic forms of hearing loss by repairing or replacing defective genes responsible for cochlear function. Additionally, advancements in neuroprosthetics aim to develop more sophisticated devices that interface directly with the brain’s auditory pathways, possibly restoring more natural hearing experiences.
Stem cell therapy is also being investigated as a means of regenerating damaged hair cells in the cochlea, offering hope for those previously deemed untreatable. Furthermore, researchers are exploring pharmacological options to prevent hearing loss caused by ototoxic substances or loud noise exposure, providing avenues for proactive protection against further degradation of auditory capabilities.
As societies increasingly recognize the importance of auditory health, future research directions emphasize multidiscipline approaches combining auditory science, engineering, and psychological aspects of communication. The prospect of individualized treatments and preventive measures heralds a new era in the management of sensorineural hearing loss, ultimately driving forward the mission of not just addressing hearing deficits but enhancing overall quality of life for those affected.